[Weekender] How South Korea went from ‘test, trace, treat’ to ‘let it spread’
Omicron revives talk of herd immunity
By Kim ArinPublished : Feb. 4, 2022 - 13:04

South Korea is determined to go easy on omicron, which is behind the ongoing record surge in COVID-19 patients, in the hope that the new dominant variant will not be as bad as the ones that came before.
But is this reckless?
The rationale for the shift to the omicron response plan is that the new variant is less threatening than its predecessor, delta, the government says.
Messaging from health officials surrounding omicron has been consistently hopeful.
Son Young-rae, spokesperson for the Ministry of Health and Welfare, has said that “half of omicron infections are asymptomatic.”
“So far omicron poses no cause for alarm,” he has said in several public appearances, including official briefings. “Omicron is shown to be only one-fifth as lethal as delta.”
He said the transition was further justified by the sharp increase in hospital capacity. The critical care bed count in the country has been expanded twofold to over 2,300, compared to before the devastating surge in December.
The director of the National Institute of Health, Kwon Jun-wook, has said that if omicron is found to be as mild as early reports suggest, there may come a point over the year when masks are no longer mandatory, except around vulnerable people.
On top of the reassurances, references to “herd immunity,” a term that had faded out of the government’s COVID-19 discourse since the ascent of the delta variant, have made a comeback.
Son said in a Jan. 25 radio interview that the herd immunity phenomenon was occurring in countries hit earlier by omicron, and that it could be a possibility for Korea.
As a milder virus assumes dominance, intense social distancing should be a thing of the past, he said. With the omicron strategy, Korea departs from its rigorous virus containment model of 3T -- “test, trace and treat” -- and moves to what has been termed a “focused protection” approach.
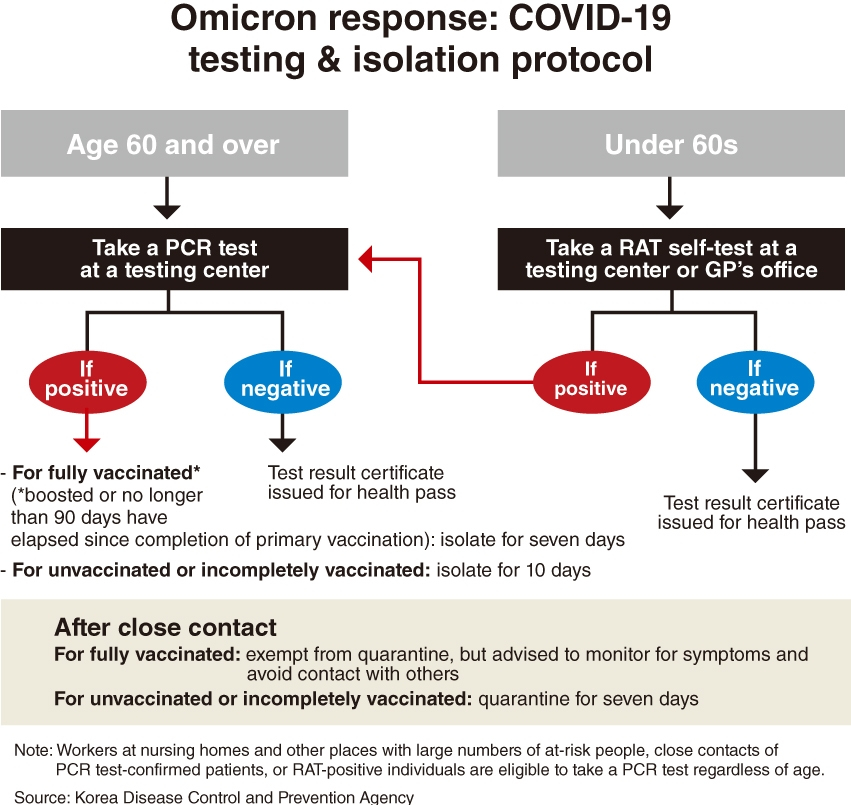
The new strategy includes restricting the most accurate PCR testing to select groups, cutting hospital stays and quarantines, putting general practitioner offices in charge of care for nonhospitalized patients and letting people contact trace themselves.
As the grip on mitigation methods eases, settings with vulnerable people like nursing homes face tighter screening, with health care workers required to be tested more frequently than before.
And although herd immunity has never been officially declared the aim, some experts suggest the plan carries such undertones.
Dr. Peck Kyong-ran, a former chief director of the Korean Society of Infectious Diseases, said in a social media statement on Jan. 24 that the omicron measures put forth so far are “prone to accelerating the spread.”
“Patients being missed by low sensitivity rapid antigen tests will go on to spread it in the community. After the shortened isolation expires, patients would still be capable of infecting others. Being doubly vaccinated doesn’t prevent people from transmitting the virus and yet they are exempt from quarantine following exposure,” she said.
“It seems like the plan is to have more in the herd become immune through infection.”
Dr. Paik Soon-young, an emeritus professor of microbiology at Catholic University of Korea, agreed that though health officials wouldn’t admit it explicitly, the new measures being implemented seemed to point to letting the virus spread naturally.
The premise underlying Korea’s plans for omicron and its implications are bringing flashbacks to the Great Barrington Declaration of October 2020, which proposed better protecting high-risk populations while letting those who aren’t as at-risk live near-normal lives as an alternative to lockdowns or “zero-COVID.”
The declaration, laid out by three scientists and endorsed by hundreds of thousands more, according to its website, sparked a heated debate then and drew criticism from public health experts.
On how and if the focused protection approach would work now that omicron is around, Dr. Jerome Kim, director general of the International Vaccine Institute, said in an email response, “The answer will be surrounded by caveats.”
He said, “We are in a much different place with regard to the virus than in October 2020, in vaccines and therapeutics.”
Success would depend on masks, distancing and frequent screening of health care workers and full vaccination -- meaning a full initial series of shots and a booster -- of the elderly and those most at risk, he said. Consideration was in order for vaccinating children, as any population that remains unvaccinated has the capacity to spread it to other people.
He called for caution against the idea of herd immunity with omicron.
“We should be cautious in assuming that omicron is the end and herd immunity will be established. Assuming that the virus is evolving for our benefit may be premature,” said the vaccine institute chief. “This is the point where we need to wait for the numbers.”
Regarding omicron, he said “it is important to point out that it is possible to be reinfected, and likely there are new strains out there that can escape prior immune responses.”
As we speak, another version of omicron, the BA.2 strain, which is even more infectious, has become dominant in Denmark and India, he said.
“Can (the BA.2 strain) infect a previously omicron infected person? Probably not, but it has 20 additional mutations not found in the original omicron and spreads 1.5 times faster.”
He went on, “The Korean government should begin to work with countries around the world to track outbreaks and variants to ensure we are not caught off-guard by ‘pi’ or ‘rho’ -- what works for omicron might not work as well for the next variant of concern.”
Paik of Catholic University of Korea said in a phone interview, “Omicron, with its astounding transmissibility, comparable to measles, forces this compromise.
“Our COVID figures are about to skyrocket. The strategy is about prioritizing so that resources go to those who need it most and systems would not be overwhelmed.”
Because access to medical services is restricted, one of the most critical challenges is monitoring and detecting rapid deterioration in patients isolating at home. As of midnight Wednesday, 97,136 patients with active infections were under home isolation, more than double the count of 42,869 seen a week prior, approaching the manageable maximum of around 109,000.
“The thing about COVID-19 is that it tends to progress very fast. Unless we can identify patients with worsening signs or symptoms quickly and get them to hospitals, we may see a bed crisis worse than the December surge in the coming month,” he said.
The front lines are not ready for a shift to the omicron strategy, health care workers say.
Hospitals are already beginning to feel the strain, according to infectious disease specialist Dr. Eom Joong-sik of Gachon University Medical Center, a government-designated COVID-19 hospital.
On the government promise that a return to strict social distancing would be a “last resort,” Eom said that steps to stall the spread “should be implemented preemptively, rather than putting it off as last resort.”
“When cases start climbing disproportionately, the choice would be down to lockdown or letting the toll fall on patients,” he said.
Primary care physician Dr. Jang Hyun-jae said although clinics were told to care for nonhospitalized patients and take on testing, no guidelines were available on how this might be done safely. “For small offices, separating infected patients from other patients is practically impossible,” he pointed out.
Perhaps the most glaring loophole in the omicron response is that patients outnumbering bed availability is already expected. Forecasts show the size of the outbreak is on course to surpass the capacity of hospitals as calculated by the government, which is based on a maximum of 50,000 patients diagnosed per day.
Dr. Jung Jae-hun, who models forecasts for the government as a COVID-19 adviser to the prime minister, said that he predicts a peak of around 100,000 new cases a day in the next five to eight weeks. In the past week, Korea has logged an average of 18,533 cases a day -- by far the highest ever recorded here.
Asked how the health care systems would hold up against an outbreak that large, Jung replied, “It wouldn’t.”
Ministry spokesperson Son admitted that after the switch to the omicron strategy, the ability to identify cases among people who are not a priority and control the spread could be undermined.
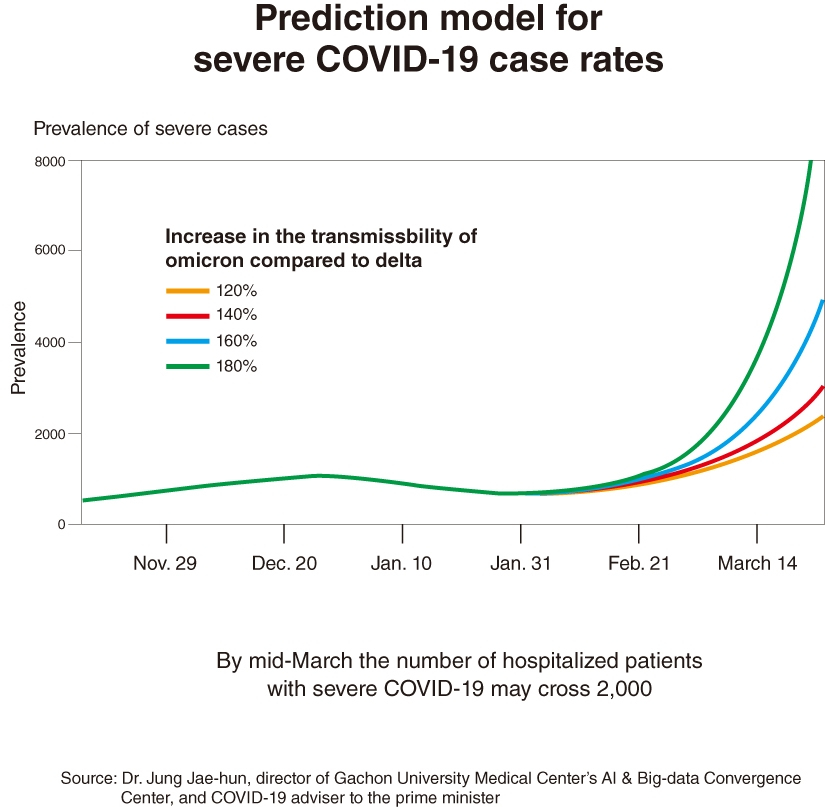
“Still, the shift is necessary. The point is to make the system more sustainable against an avalanche of cases,” Jung said, adding, omicron was turning out to be even less severe than initially calculated.
Though health officials said the Pfizer oral antiviral treatment was expected to somewhat cushion the blow, its effect had been only slight so far, mainly due to how sparsely it is being distributed.
In the two weeks after the first shipments arrived in mid-January, just 506 patients were prescribed the pill. A chief doctor at a public hospital in Seoul said the age cutoff of 60 and above and the many medications that it cannot be prescribed alongside, among other aspects, were preventing the pills from being used widely.
Dr. Kim Woo-joo, an infectious disease professor at Korea University and president of the Korean Vaccine Society, argued Korea should “at least put up a good fight -- test extensively -- before retreating to a contingency plan, because it seems it is well within our capacity.”
Recently an average of only 200,000 to 300,000 PCR tests have been carried out each day, far below the government-touted maximum capacity of 850,000.
Kim of Korea University said age-based prioritizations were neglecting people of younger ages with vulnerabilities. “The age criteria of 60 years for priority access is, if anything, too narrow. For people in their 50s the fatality rate is fairly high at around 0.3 percent.”
Though Korea is not the only country to take a more laissez-faire approach in response to omicron, it likely has larger susceptible populations because of low levels of infection until now, he said. The Korea Disease Control and Prevention Agency’s seroprevalence survey of 994 people aged 10 to 94, conducted July-October last year, showed 67 percent of them had spike protein antibodies.
“There should also be a safety net for people who are being left out of surveillance with the limited availability, like people who can’t afford the 9,000 to 16,000 won ($7.50-$13.30) at-home test kit or the 5,000 won that is now required to get a PCR test when they have symptoms,” he said.
“If we fail to address people being sidelined, we risk turning the situation into some sort of survival-of-the-fittest experiment.”
People who work with vulnerable groups question the viability of the promise of “focused protection.”
Dr. Noh Dong-hoon, director of a nursing hospital in Gyeonggi Province, pointed out that “people at higher risk, and those who work with them, do not exist in a bubble separate from the rest of the society.”
A government notice sent to nursing facilities nationwide on Jan. 26 said workers were mandated to take a PCR test two to three times a week, on top of rapid self-tests. They were to refrain from nonessential outings and gatherings in light of the dangers of asymptomatic transmission.
“Nursing (home) workers are being asked to practically limit their daily itineraries to their workplace and nowhere else, and stay isolated from families and friends,” he said. Despite the “impossible demands,” no compensation has come from the government, he added.
“The virus doesn’t discriminate. How do we stop it from getting to the more vulnerable among us?” posed Eom, who works with severely sick COVID-19 patients. “It’s not clear-cut like that.”
Kim of the International Vaccine Institute said it would be hard to protect older people who are not in nursing homes from those around them, some of whom may be asymptomatic. “In a sense then the elderly become ‘canaries,’” he said.
But does the altered strategy mean Koreans will have more freedom? Not necessarily, according to Jang Young-ook, a researcher at the Korea Institute for International Economic Policy studying pandemic response policies among countries.
While the omicron plan is big on cutting down on administrative burdens, on an individual level the scope of freedom has not been expanded greatly, at least for the time being, he said. A cap on the size of social gatherings and nighttime curfews remain in place at least until Sunday. The mask mandate is also not going away anytime soon and QR code passes continue to be a requirement at most public places.
The omicron strategy is “a declaration that society will no longer devote its resources to stopping the virus from spreading,” he said. “This, of course, must only proceed under the scenario that medical systems are able to handle the patient influx without collapsing.”
Jang went on, “Such significant changes in policy are best preceded by efforts to build consensus through open, public conversations -- something that has been lacking.”
“The less the government shoulders responsibility for individual sickness, the fewer grounds there are for state interventions in personal behavior,” he said.
By Kim Arin (arin@heraldcorp.com)









![[Hello India] Hyundai Motor vows to boost 'clean mobility' in India](http://res.heraldm.com/phpwas/restmb_idxmake.php?idx=644&simg=/content/image/2024/04/25/20240425050672_0.jpg&u=)









