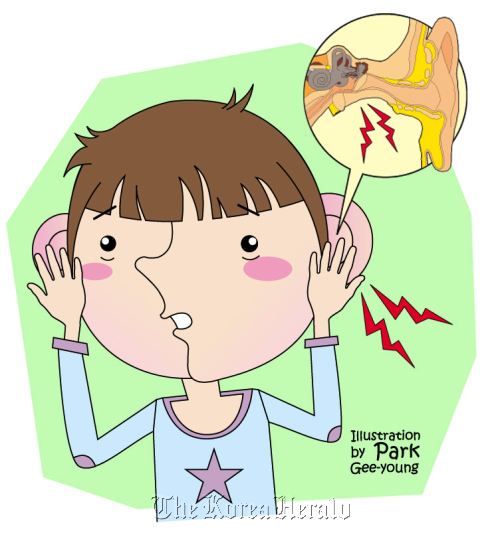
Otitis media refers to all types of inflammation of the middle ear caused by an infection.
It is the second most frequently diagnosed disease among outpatients of otorhinolaryngology and pediatrics, following upper respiratory tract inflammation.
About one-third of infants aged 3 and under suffer from acute otitis media at least three times, and two-thirds at least once. Some infants are found to develop sequelle from this condition. Cases of fatal complications have been dramatically reduced due to the advancement of antibiotics.
However, severe complications are still seen in rare cases, and complications such as conductive hearing loss are actually increasing.
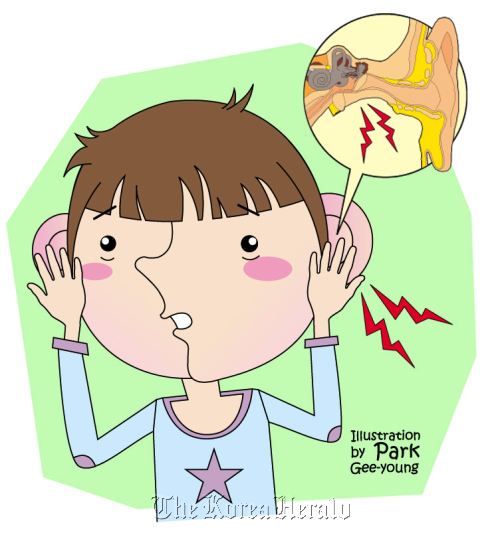
Chronic middle ear infection may lead to conditions such as perforation of the eardrum, adhesive otitis media, tympanosclerosis, and fixation or discontinuity of auditory ossicles. Inflammation of the middle ear is categorized into three types in accordance with its duration: acute if lasting up to three weeks, subacute if lasting between three weeks and three months, and chronic if lasting three months or longer.
By symptoms, inflammation of the middle ear is mainly categorized into acute otitis media associated with fever, pain, inflammation of the eardrum, and effusion; chronic serous otitis media often featuring fluid accumulation without any pain, a feeling of fullness in the ear, and inflammation of the eardrum; and chronic suppurative otitis media characterized by perforation of the ear drum and drainage.
Chronic suppurative otitis media can be further classified into cholesteatomatous otitis media and non-cholesteatomatous otitis media. Acute otitis media and serous otitis media are commonly diagnosed among infants because an infant’s Eustachian tube is smaller and shorter than an adult’s. Young children’s Eustachian tubes are also positioned more horizontally, with more lymphatic tissue within the nasopharyngeal cavity. Thus, they are more susceptible to becoming blocked by swelling in the case of an upper respiratory tract infection.
I would like to focus on chronic suppurative otitis, of which adults are at greater risk.
Chronic suppurative otitis media
Chronic suppurative otitis media is a term used to describe a variety of symptoms of long-term inflammation, such as perforation of the eardrum and drainage (pus and discharges) from the middle ear and the mastoid air cells. When acute otitis media is not resolved properly and inflammation persists, middle ear effusion (fluid behind the eardrum) occurs and the mucosa and bony structure of the middle ear become irreversibly damaged, thus causing chronic otitis media.
While the patient chronic otitis media experiences no pain, they do experience the buildup of pus or discharges and hearing loss. In particular, cholesteatomatous otitis media often accompanies an odor, as well as pulsatile drainage when associated with acute inflammation. Suppurative otitis media is normally a condition devoid of pain and nausea. If such symptoms are present, it may indicate the onset of complications.
The ultimate goals of chronic otitis media treatment are: the removal of inflammation; the prevention of inflammation recurring; hearing improvement; and the prevention of further complications. Oral administration and injection of different antibiotics may reduce drainage and ease inflammation, but these methods are insufficient in fully eliminating the problems and restoring hearing.
Therefore, surgery is typically recommended. If inflammation has rapidly progressed and led to severe drainage, the external auditory canal and inflamed middle ear space must first be thoroughly cleaned, then antibiotic susceptibility testing should be performed, and finally appropriate antibiotics should be administered accordingly.
Antibiotic eardrops may be applied additionally. Some patients clog the ear with cotton balls or apply untested home remedies in an attempt to block drainage, which only exacerbates inflammation and may even result in hearing loss due to the toxicities of drugs used.
The most commonly performed surgeries include mastoidectomy and tympanoplasty. The former involves the removal of infected or damaged parts of the bony mastoid process. The latter is an operation for the reconstruction of the damaged eardrum using autologous soft tissues taken from around the ear (the temporalis fascia or the perochondrium). In most cases, the eardrum heals within one or two months of surgery. In 95 percent of cases, surgery results in a dry, healthy ear and successfully restored hearing.
It is the second most frequently diagnosed disease among outpatients of otorhinolaryngology and pediatrics, following upper respiratory tract inflammation.
About one-third of infants aged 3 and under suffer from acute otitis media at least three times, and two-thirds at least once. Some infants are found to develop sequelle from this condition. Cases of fatal complications have been dramatically reduced due to the advancement of antibiotics.
However, severe complications are still seen in rare cases, and complications such as conductive hearing loss are actually increasing.
Chronic middle ear infection may lead to conditions such as perforation of the eardrum, adhesive otitis media, tympanosclerosis, and fixation or discontinuity of auditory ossicles. Inflammation of the middle ear is categorized into three types in accordance with its duration: acute if lasting up to three weeks, subacute if lasting between three weeks and three months, and chronic if lasting three months or longer.
By symptoms, inflammation of the middle ear is mainly categorized into acute otitis media associated with fever, pain, inflammation of the eardrum, and effusion; chronic serous otitis media often featuring fluid accumulation without any pain, a feeling of fullness in the ear, and inflammation of the eardrum; and chronic suppurative otitis media characterized by perforation of the ear drum and drainage.
Chronic suppurative otitis media can be further classified into cholesteatomatous otitis media and non-cholesteatomatous otitis media. Acute otitis media and serous otitis media are commonly diagnosed among infants because an infant’s Eustachian tube is smaller and shorter than an adult’s. Young children’s Eustachian tubes are also positioned more horizontally, with more lymphatic tissue within the nasopharyngeal cavity. Thus, they are more susceptible to becoming blocked by swelling in the case of an upper respiratory tract infection.
I would like to focus on chronic suppurative otitis, of which adults are at greater risk.
Chronic suppurative otitis media
Chronic suppurative otitis media is a term used to describe a variety of symptoms of long-term inflammation, such as perforation of the eardrum and drainage (pus and discharges) from the middle ear and the mastoid air cells. When acute otitis media is not resolved properly and inflammation persists, middle ear effusion (fluid behind the eardrum) occurs and the mucosa and bony structure of the middle ear become irreversibly damaged, thus causing chronic otitis media.
While the patient chronic otitis media experiences no pain, they do experience the buildup of pus or discharges and hearing loss. In particular, cholesteatomatous otitis media often accompanies an odor, as well as pulsatile drainage when associated with acute inflammation. Suppurative otitis media is normally a condition devoid of pain and nausea. If such symptoms are present, it may indicate the onset of complications.
The ultimate goals of chronic otitis media treatment are: the removal of inflammation; the prevention of inflammation recurring; hearing improvement; and the prevention of further complications. Oral administration and injection of different antibiotics may reduce drainage and ease inflammation, but these methods are insufficient in fully eliminating the problems and restoring hearing.
Therefore, surgery is typically recommended. If inflammation has rapidly progressed and led to severe drainage, the external auditory canal and inflamed middle ear space must first be thoroughly cleaned, then antibiotic susceptibility testing should be performed, and finally appropriate antibiotics should be administered accordingly.
Antibiotic eardrops may be applied additionally. Some patients clog the ear with cotton balls or apply untested home remedies in an attempt to block drainage, which only exacerbates inflammation and may even result in hearing loss due to the toxicities of drugs used.
The most commonly performed surgeries include mastoidectomy and tympanoplasty. The former involves the removal of infected or damaged parts of the bony mastoid process. The latter is an operation for the reconstruction of the damaged eardrum using autologous soft tissues taken from around the ear (the temporalis fascia or the perochondrium). In most cases, the eardrum heals within one or two months of surgery. In 95 percent of cases, surgery results in a dry, healthy ear and successfully restored hearing.

By Cho Yang-sun
The author is a professor of Otorhinolaryngology-Head and Neck Surgery at Sungkyunkwan University School of Medicine. ― Ed.
-
Articles by Korea Herald



![[Herald Interview] 'Amid aging population, Korea to invite more young professionals from overseas'](http://res.heraldm.com/phpwas/restmb_idxmake.php?idx=644&simg=/content/image/2024/04/24/20240424050844_0.jpg&u=20240424200058)










![[KH Explains] Korean shipbuilding stocks rally: Real growth or bubble?](http://res.heraldm.com/phpwas/restmb_idxmake.php?idx=652&simg=/content/image/2024/04/25/20240425050656_0.jpg&u=)

